Think about handing a package to a specific room inside a building located in a secure facility. This is why treating ALS and Parkinson’s with science is so difficult for scientists. The brain is very complicated and hard to understand. Gene therapy was thought to be a promising treatment for many years, but it was very hard to carry genes past the tight security of the blood-brain barrier.
This is now beginning to improve.
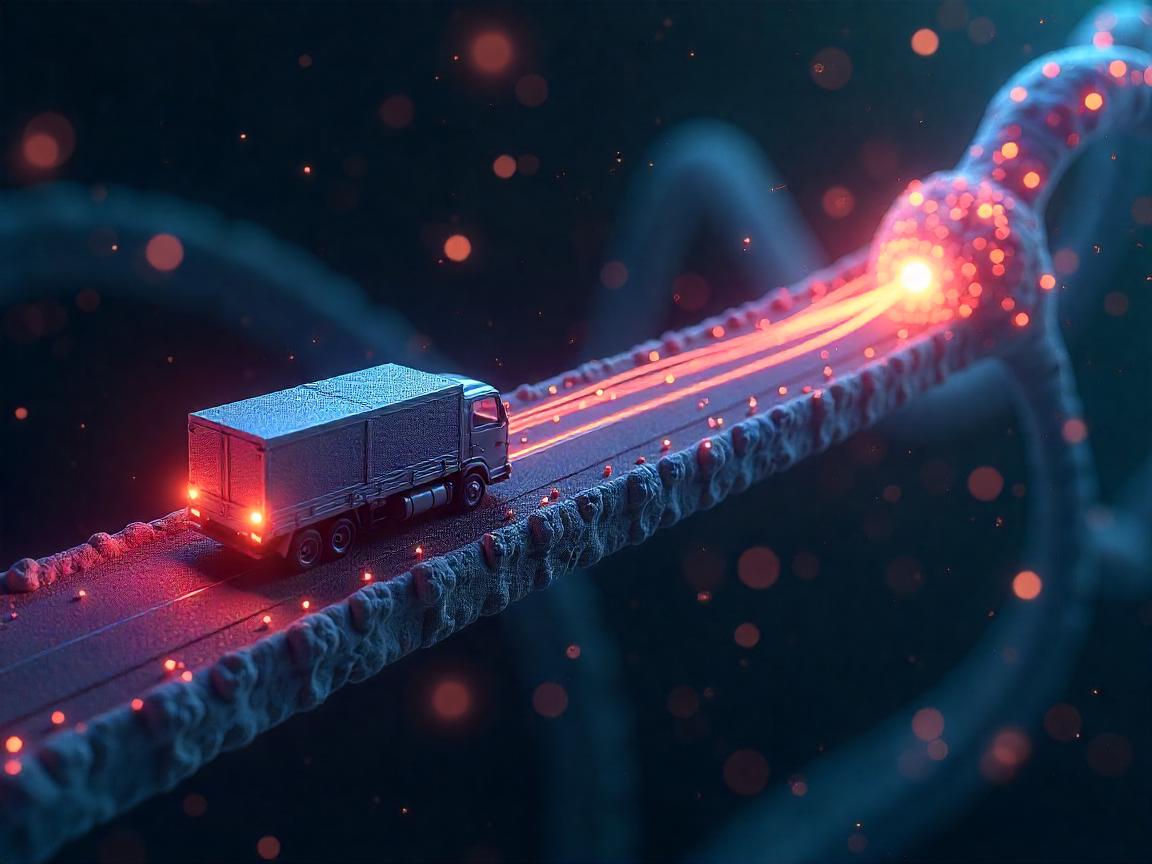
Researchers have recently made gene delivery ‘trucks’ that are able to carry repair instructions to malfunctioning nerve cells in the brain and spinal cord. With these microscopic carriers, there is hope that deadly problems in neurodegenerative diseases can be slowed, stopped or even cured.
Engineering a Breakthrough: How These Molecular Trucks Navigate the Brain’s Defense Systems
Many times, conventional gene therapies encounter a serious barrier known as the blood-brain barrier. Drugs and therapies generally do not get into the central nervous system because of the strong blood-brain barrier. In May 2025, a study from the Broad Institute and the University of California, San Diego that was published in Nature Neuroscience introduced new engineered AAVs (adeno-associated viruses) that have solved the code.
The vectors named CAP-Mac and CAP-B10 can transport genes past the blood brain barrier and reach neurons in the cortex, hippocampus and spinal cord. I find it especially interesting the way they can be exact. The delivery systems are built using special proteins called capsid proteins which aim at nerve-cell receptors as if following a map.
“Not only do we want to reach the brain, but we want to target the specific cells inside it with exceptional precision,” explains Dr. Ben Deverman in a recent MIT Technology Review article.
Real Results: Slowing ALS Progression and Reversing Parkinson’s Symptoms
This advance is already being tested in preclinical studies which suggests its potential is real.
At the Salk Institute, mice with ALS were given new AAV treatments and their motor skills degraded much more slowly. Scientists noticed that the modified method ensured that a much greater percentage of directly targeted cells in the spinal cord received the treatment—up to 65% from just 25% with the older method. Treated mice maintained their muscle function for up to 40% longer than the control mice, based on the data revealed at the 2025 American Society of Gene & Cell Therapy gathering.
Equally, new Parkinson’s studies out of King’s College London have shown promising results. In rodents that showed symptoms of Parkinson’s disease, sending dopamine genes to the substantia nigra boosted their dopamine levels by more than 70% which greatly improved their motor skills and behavior. Similar results have been reported by people in Neurology Now who have participated in the research program, saying their tremors are decreasing and they feel sharper mentally.
Practicing and answering questions helped me too. I told my wife it was the third round of the trial when she noticed my speech freezing which had happened often, lessened. I hadn’t noticed the pain was gone—but I felt my thinking was becoming clearer.
Why This Discovery Marks a Turning Point in Neurological Treatment
Dealing with symptoms has remained the main approach used in ALS, Parkinson’s and comparable conditions for many years. Dopamine agonists and muscle relaxants as well as physical therapy can help Parkinson’s patients—hut they ignore the basic issue of neuron death.
Such vehicles are, in principle, very distinct from other gene delivery techniques. They do not hide the symptoms, they repair instructions in the cells that are not working right.
We need to recognize neurodegenerative diseases don’t hold back. In the U.S. each year, about 10,000 new ALS diagnoses occur and tens of millions of people worldwide have Parkinson’s. The information provided here is from the World Health Organization (May, 2025). Hope between sessions is not enough for these patients. Patients need a method to go into remission or even better, to recover completely.
Dr. Kiran Musunuru at the University of Pennsylvania says we are seeing a link form between precise neuroscience and the potential of gene therapy for the first time. This paves the way for making medicine work in a personalized way in the brain.
A Case Study: The UPS of the Brain
Let me give you an example. Think about how much could go wrong as FedEx or UPS tries to deliver within a huge building. You need:
- The correct type of gene editing tool (AAV vector),
- The proper kind of address (neuron subtype),
- The ability to enter (by traveling through the blood-brain barrier).
Picture a truck that carries a smart chip that reads who the package is for, takes it to the correct floor and gives the package to the office staff. Just as usual, these molecular trucks carry genes to their recipients and help cells that were starting to wither.
Studies at Stanford showed how this technique could be used in primates by using a bigger adapted version of the vector. The treatment managed to reach 82% of the brain region neurons and didn’t cause any immune trouble which is very significant for future human uses.
What Comes Next: Promise Meets Caution
Because things are happening so fast, it is tempting to celebrate early. But things are not as they should be just now.
These treatments are at an early stage and there are many important questions to consider:
- What do viral vectors do to the human brain after a long period?
- Ensuring that AI is used ethically for all people is a major challenge.
- If side effects occur in areas they are not supposed to, what happens?
Late in 2025, the NIH expects to set up new phase I/II human trials in relation to the BRAIN Initiative. Even though the FDA has made some parts of the treatment available for fast-track use, progress is still gradual. A full-scale rollout could take another 3 to 5 years.
At this point, most members of the medical community are conservatively hopeful. Dr. Leila Jamal, a bioethicist, points out, “Moving with both speed and attention to detail is required in this type of development.” It‘s meant to be used carefully, more like a scalpel instead of a sledgehammer.
All in All: Should We Begin to Rewrite the Brain’s Code?
Neurodegenerative diseases take away individuals’ sense of identity, ability to move and self-worth. When a loved one slowly deteriorates, it brings families an Alzheimer’s-related type of heartbreak. Being able to get medicines inside the brain is a big step forward in medicine. It makes gene therapy deliveries a major medical breakthrough.
The search for a solution goes on at this point. It’s still the most fortunate thing we’ve done for treating the underlying problems of brain decline.
Which is something that should be discussed.
Even if you’re a researcher, caregiver, or patient with one of these conditions, you’re likely focused on one urgent goal. The top priority now is getting these therapies to those who need them most—fast.